 Authored by Beth Umland, Director of Employer Research for Health and Benefits, Mercer
Authored by Beth Umland, Director of Employer Research for Health and Benefits, Mercer
More than 1,300 organizations have completed Version 4 of the HERO Health and Well-Being Best Practices Scorecard in Collaboration with Mercer since it was launched in 2014. As we prepare to move on to Version 5 of the Scorecard early next year, we decided to delve into the robust data we have collected over the six years that Version 4 has been in the field to examine the prevalence of a number of key strategies and how their use has changed over time.
For this analysis, we compared Scorecard data submitted between 2014-2016 and data collected between 2018-2020. (For simplicity, we refer to the earlier dataset as 2016 and the current dataset as 2020.) We restricted the analysis to employers with 5,000 or more employees, for two reasons. Employers of this size tend to be the early adopters of health and well-being initiatives, as well as role models for smaller employers. In addition, because the 2020 dataset includes substantially more small employers than the 2016 (the average number of employees was 5,931 in 2016 but only 4,688 in 2020), restricting the analysis to a defined size group reduces the “noise” created by shifting demographics across the two samples being compared. The 2016 dataset includes 148 employers with 5,000 or more employees and the 2020 dataset includes 115.
Whether organizations decide to invest in health and well-being initiatives or not depends, at least to a certain extent, on whether these investments are seen as contributing to business results. Scorecard results suggest there is growing consensus on this point. Respondents are asked whether the leaders of their organization understand the strategic importance of employee health and well-being: “To what extent is your program viewed by senior leadership as connected to broader business results?” Those responding “to a great extent” rose from 22% in 2016 to 30% in 2020 (the most common response in both years was “to some extent”).
How has this growing recognition of the importance of health and well-being translated to action? To gauge the adoption of the most meaningful practices over time, this longitudinal comparison focuses on the four clusters of practices that emerged from a factor analysis as having a strong, statistically significant effect on Scorecard completers’ perceptions about the effectiveness of their workplace health and well-being initiatives1:
- Organizational and Leadership Support
- Incentives
- Program Integration
- Program Comprehensiveness
Organizational and leadership support
A recent HERO study found that Organizational and Leadership Support practices are the most highly predictive of positive health and well-being outcomes such as program participation, health and medical cost impact, and employee perceptions of organizational support.2
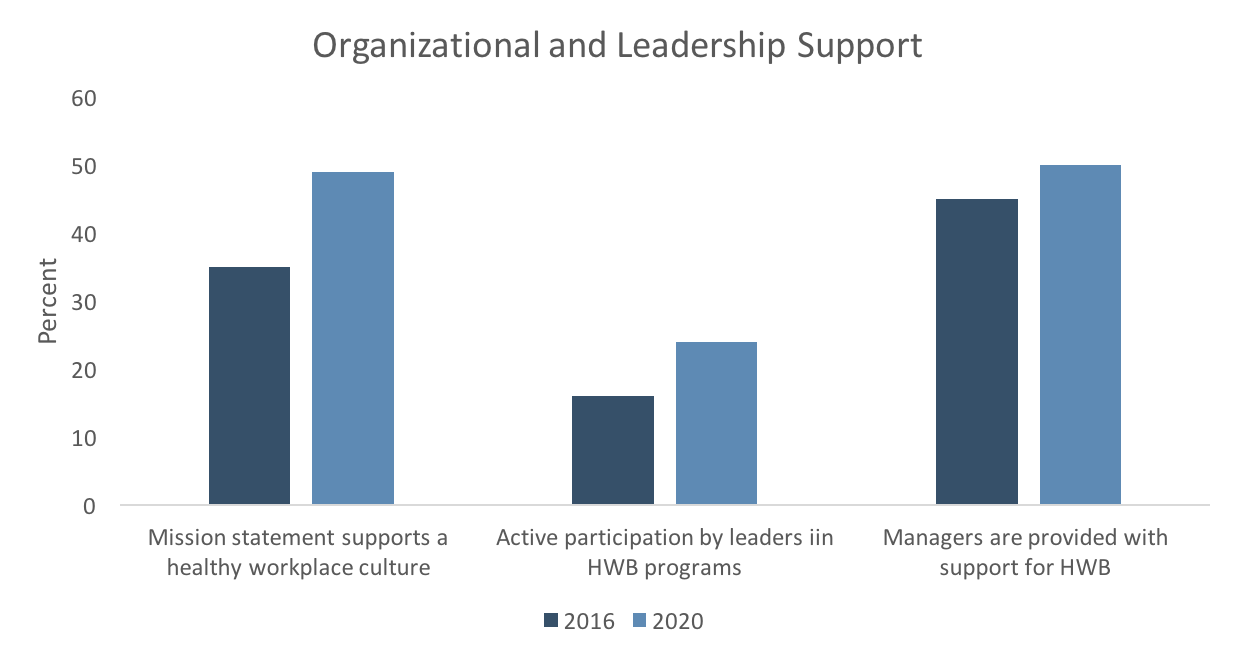
The HERO Scorecard asks detailed questions about organizational support strategies. One important way for an organization to demonstrate commitment to, and maintain focus on, employee well-being is with the company vision or mission statement. Scorecard respondents reporting that their company vision or mission statement supports a healthy workplace culture jumped from 35% in 2016 to 49% in 2020.
One of the practices found to have a strong influence on outcomes in the recent study is active participation by leaders in health and well-being programs. However, there was no change in this best practice from 2016 to 2020 – in each dataset, 51% of respondents said leaders actively participate. There was some improvement in leaders acting as role models for prioritizing health and work/life balance (for example, by taking activity breaks during the day, not sending email while on vacation, and so on), from 16% in 2016 to 24% in 2020, but even so, this best practice is still far from the norm.
However, more companies are committing to providing managers and supervisors with training, budget, and resources that allow them to support well-being. In 2020, 50% of respondents say mid-level managers are given some or a lot of support, up from 45% in 2016.
Programs
A slightly smaller percentage of employers are assessing employee heath with health assessments and biometric screenings in 2020 (77% and 74%, respectively) than were doing so in 2016 (87% and 78%, respectively). At the same time, there has been a slight increase in claims data mining (from 78% to 82%) and in the use of monitoring or tracking devices to assess employee health (from 29% to 33%).
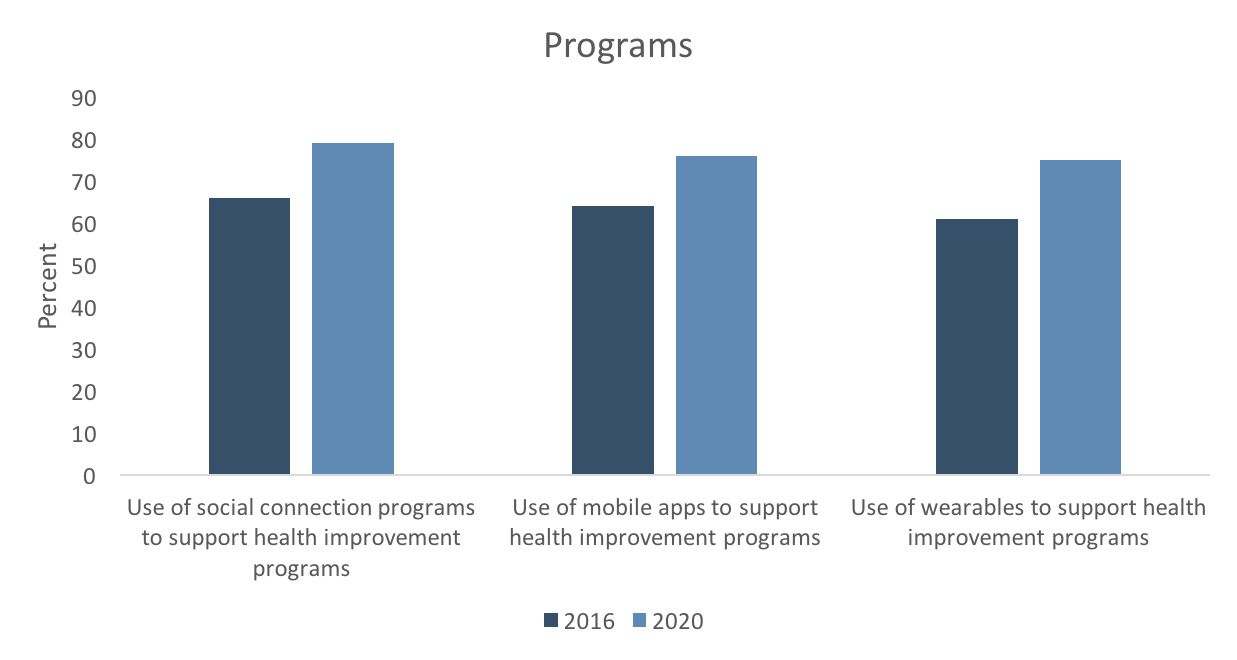
Not surprisingly, there has been rapid growth in the use of technology to support health improvement programs, such as wearables (from 61% to 75%), mobile apps (64% to 76%) and social connection programs (from 66% to 79%). HERO Scorecard data has shown that participation rates are higher among employers using technologies that create a more personalized, real-time experience3 – and participation rates are a leading indicator of program effectiveness.
Program integration
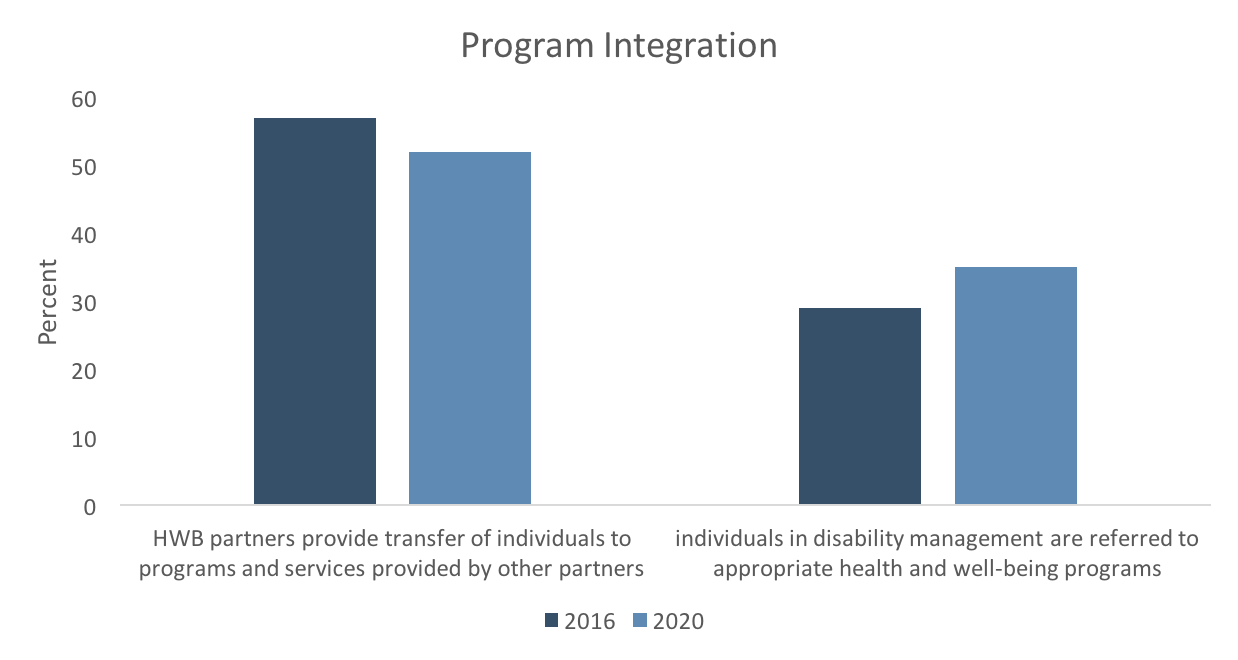
Respondents in the 2020 database still have plenty of room for improvement in terms of ensuring that their health and well-being programs are effectively integrated with each other, the health plan, the safety program, and disability programs. In 2020, just 52% of respondents said that “Health and well-being partners provide warm transfer of individuals to programs and services provided by other partners” — and this is down from 57% in 2016. This trend is concerning because HERO Scorecard data suggest that program integration positively influences program effectiveness.1,4
There was a modest increase (from 29% to 35%) in respondents reporting that individuals in disability management are referred to appropriate health and well-being programs. Lack of integration in this area seems to be a missed opportunity given that employees may be more ready to engage in health programs at a time when they are struggling with a significant health issue. In addition, employer support during a time of employee illness or injury may positively influence employee attitudes about returning to work.5
Incentives and other participation strategies
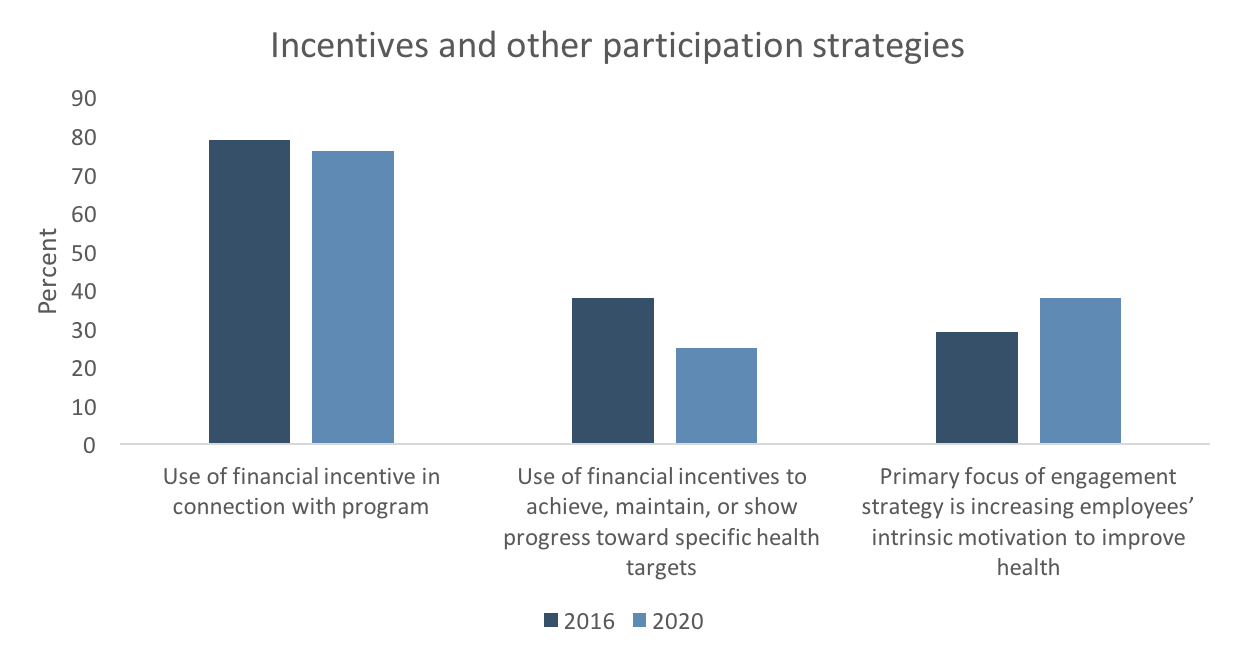
Participation strategies include incentives, communication and education. Of these, financial incentives seem to have the most direct influence on participation rates and affect program outcomes. However, while the majority of 2020 respondents (76%) use some type of financial incentive in connection with their programs, this is down slightly from 79% in 2016. Further, the use of financial incentives to achieve, maintain, or show progress toward specific health status targets (“outcomes-based incentives” as opposed to participatory incentives) has fallen sharply, from 38% in 2016 to 25% in 2020. While Scorecard data do not help us understand the reasons for this trend, it might be due to increasing employer concerns about the permissibility of these types of incentives.6
The median maximum value of all participatory incentives that a member can earn is $500 in 2020, up just slightly from $449 in 2016. Respondents in 2020 report that, on average, 55% of eligible employees earn at least some of the available incentive and 38% earn the maximum incentive, little changed from 2016.
While financial incentives are still widely used, there was an increase in respondents saying that increasing employees’ intrinsic motivation to improve or maintain their health is the primary focus of their engagement strategy, from 29% in 2016 to 38% in 2020. In addition, the already-strong focus on communication to drive engagement continues to build. In 2020, 81% of respondents have branded the health and well-being program with a unique name and logo, up from 77% in 2016; the use of regular status reports to inform stakeholders of progress has risen to 57% from 53%; and communications directed to spouses and family members as well as employees has risen to 44%, from 41%.
In the next version of the HERO Scorecard, as in the past updates, we have been guided by analyses of Scorecard data as well as by input from experts in the field. While Version 5 will offer a number of new practices for employers to consider, some of the Version 4 practices will be retired. However, the practices discussed above have demonstrated their continued importance and will, we hope, continue to spread.
HERO would like to thank and acknowledge the following HERO Scorecard commentary reviewers: David Anderson (VisioNEXT, LLC), Kerry Evers (Pro-Change Behavior Systems), Stefan Gingerich (StayWell/WebMD Health Services), Jessica Grossmeier (HERO), Mary Imboden (HERO), and Steven Noeldner (Mercer).
References
- Imboden M, Castle PH, Johnson SS, Rahrig-Jenkins K, Pitts JS, Grossmeier J, Mangen DJ, Mason S, Noeldner SP. Development and validity of a workplace health promotion best practices assessment. Journal of Occupational and Environmental Medicine. 2020;62(1):18-24.
- Grossmeier J, Castle PH, Pitts JS, Saringer C, Jenkins KR, Imboden MT, Mangen DJ, Johnson SS, Noeldner SP, Mason ST. Workplace well-being factors that predict employee participation, health and medical cost impact, and perceived support. American Journal of Health Promotion. 2020;34(4):349-358.
- Harvey M. Can technology drive engagement in wellness programs? HERO Scorecard Commentary. August 22, 2016. Available at: https://hero-health.org/blog/can-technology-drive-engagement-in-wellness-programs/
- Saringer C. Assessing the influence of leadership commitment and program integration. HERO Scorecard Commentary. August 20, 2019. Available at: https://hero-health.org/blog/assessing-the-influence-of-leadership-commitment-and-program-integration/
- Buys NJ, Selander J, Sun J. Employee experience of workplace supervisor contact and support during long-term sickness absence. Disability and Rehabilitation. 2019 Apr;41(7): 808-814.
- Pollitz K, Rae M. Trends in workplace wellness programs and evolving federal standards. KFF. June 9, 2020. Available at: https://www.kff.org/private-insurance/issue-brief/trends-in-workplace-wellness-programs-and-evolving-federal-standards/
Data cited in this commentary are based on the US version of the HERO Scorecard v4 responses, submitted through June 30, 2020.
